Redesigned Blues Brief available electronically
Blues Brief has a new look, and now you can subscribe to it electronically. Visit bcbsm.com/providers, click Our Provider Newsletters and then the green Subscribe button. Choose from Blues Brief for hospitals and facilities as well as other new specialty-specific versions. Read more on Page 7 of the January–February 2019 BCN Provider News.
2019 products at a glance flyers available
These flyers are general summaries of Blue Cross and BCN products, including the product name, prefix and brief description. These flyers can be found on the BCN Provider Publications and Resources web-DENIS page under BCN Products or the BCBSM Newsletters and Resources web-DENIS page under Products and Networks.
Finding your products guide now available
This new step-by-step guide shows you how to “find yourself” using the Blue Cross online provider search on bcbsm.com so you can confirm which Blue Cross and BCN products you accept. It can be found on web-DENIS on the BCBSM Newsletters and Resources page under Products and Networks as well as BCN Provider Publications and Resources under BCN Products.
BCN continues Behavioral Health Incentive Program in 2019
The BHIP offers broad-based suggestions for implementing practices shown to improve the well-being of patients and to reward those initiatives. The BHIP booklet and flyer will be available on web-DENIS starting in January. Read more on Page 20 of the January–February 2019 BCN Provider News.
Reminder: FEP made changes to care admissions request for skilled nursing facility
Since April 30, 2018, all post-acute care admissions, including skilled nursing facilities, have been routed to the Precertification Utilization Management team. Federal Employee Program members must sign a consent for case management to use their benefit for a skilled nursing facility. If an FEP member has Medicare Part B, and also has Medicare Part B services on the claim, then that claim must be submitted to Medicare for processing before FEP can process the claim.
For additional information, see the November 2018 issue of The Record.
FEP billing guidelines for physical, speech and occupational therapy at skilled nursing facilities
For a list of guidelines to use when billing for physical, speech and occupational therapy at SNFs for Federal Employee Program members, see the October 2018 issue of The Record.
Pharmacy updates
New user-friendly prompts coming to Pharmacy Prior Authorization Help Desk
See the October 2018 issue of The Record.
AllianceRx Walgreens Prime specialty pharmacy program starts Jan. 1
See Page 29 of the January–February 2019 BCN Provider News or the November 2018 issue of The Record.
ESI to be Michigan retail pharmacy network manager for our commercial business, starting Jan. 1
See the December 2018 issue of The Record.
URMBT members with Medicare Plus Blue to receive fifth-level hospice services
Beginning Jan. 1, 2019, UAW Retiree Medical Benefits Trust members with Medicare Plus Blue will be eligible to receive fifth-level hospice benefits which covers inpatient room and board in a skilled nursing facility. There’s a lifetime maximum of 210 days of coverage for fifth-level care.
For additional benefits and billing information, see the December 2018 issue of The Record.
Changes for UAW Retiree Medical Benefits Trust non-Medicare members
Beginning Jan. 1, the UAW Retiree Medical Benefits Trust Traditional Care Network and PPO plans will transition to the Enhanced Care Plan (ECP) for non-Medicare UAW hourly auto retirees (only). This plan features health management programs that include prior authorization requirements for medical oncology, radiation oncology and specialty drugs.
For additional information, see the December 2018 issue of The Record.
Change to prior authorization requirement for PPO members
In an October 2018 issue of The Record, we told you that you’d need to obtain prior authorization for high-tech radiology, in-lab sleep management and echocardiogram services for all Blue Cross Blue Shield of Michigan PPO members, regardless of where they lived. We’ve subsequently changed our approach and will only require prior authorization for those services for patients who live in Michigan.
GM to offer new PPO plan option - ConnectedCare: Henry Ford Health System
Effective Jan. 1, General Motors will offer a new PPO medical plan option for select salaried employees and eligible dependents in the Detroit area called ConnectedCare: Henry Ford Health System (group number 83640). Please note that this plan option is not affiliated with BCN AdvantageSM HMO ConnectedCare.
Blue Cross will serve as the third-party administrator of benefits for this plan option. As always, you can check web-DENIS for patient benefit and eligibility information.
For additional plan information, see the December 2018 issue of The Record.
e-referral now includes updated authorization criteria and questionnaires
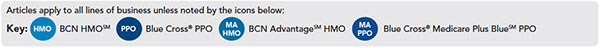
We’ve made updates to the authorization criteria and questionnaires in the e-referral system for several procedures. We use these criteria and questionnaires when making utilization management determinations for BCN HMO, BCN Advantage, and Blue Cross Medicare Plus Blue PPO members.
For more information, see the December 2018 issue of The Record.