
|
|---|
|
|
| This newsletter includes short summaries, reminders and updates for Blue Cross and BCN providers. Please visit The Record or BCN Provider News for complete newsletter editions. BCN no longer accepts referrals for BCN Advantage members staying in network Effective March 2019, Blue Care Network no longer accepts referrals for BCN Advantage℠ members to see a provider in their health plan’s network. These referrals are no longer needed. Authorizations and plan notifications are still required for certain services. For more information, see Page 7 of the March–April 2019 BCN Provider News. Reminder: New clinical editing system changes Although we’ve delayed our upgrade to a new clinical editing system — from ClaimCheck to ClaimsXten — we want to remind you about key changes. Please see the explanation of changes with new explanation codes and the clinical editing form on Page 27 of the March–April 2019 BCN Provider News. Complete new questionnaires in e-referral for BCN members New questionnaires are open for BCN authorization requests in the e-referral system for the following outpatient procedures:
In addition, updated or new questionnaires for the following services opened for BCN authorization requests in the e-referral system on Nov. 25, 2018:
We’ve made preview questionnaires available at ereferrals.bcbsm.com. To find them, click BCN, then click Authorization Requirements & Criteria. Next, look in the "Authorization criteria and preview questionnaires" section. For more information, see Page 31 of the March–April 2019 BCN Provider News. Sign up to receive Blues Brief electronically As announced previously, Blues Brief has a new look and is now available via email subscription. To sign up and avoid possible subscription errors, add Blues Brief to your subscriptions by clicking the Manage Subscriptions link at the bottom of your BCN Provider News or The Record newsletter emails. You can also visit the subscription page on bcbsm.com/providers to choose your preferred Blues Brief versions. Read more on Page 6 of the March–April 2019 BCN Provider News or the March 2019 issue of The Record. Prior authorization changes coming to AIM authorization program Beginning May 1, 2019, the PPO radiology management program, administered by AIM Specialty Health, will be adding a cardiology and in-lab sleep study prior authorization program for Medicare Plus Blue PPO members. This includes UAW Retiree Medical Benefits Trust members with Medicare Plus Blue coverage. For more information, see the February 2019 issue of The Record. We’re removing providers on the CMS preclusion list from our commercial and MA networks In January, we notified providers that we’re required by the Centers for Medicare & Medicaid Services to remove providers from our Medicare Advantage networks if they are on the CMS preclusion list. We are also removing providers who are on the CMS preclusion list from all Blue Cross Blue Shield of Michigan commercial and Blue Care Network HMO provider networks. These providers will be removed from our online provider directories, and providers on the preclusion list won’t be permitted to enroll in any of our commercial or Medicare Advantage networks. For more information about the CMS preclusion list, go to cms.gov** and type Preclusion list in the search box. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. DME/P&O telehealth prescription restrictions don’t include CPAP devices In October 2018, we reported that members can no longer receive prescriptions for DME or P&O items through telehealth visits. This doesn't apply to CPAP devices. (Blue Cross will continue to cover medically necessary DME items ordered by providers after face- to-face visits.) PPO Northwood to cover DME/P&O utilization management and claims starting in May Beginning with dates of service on or after May 1, 2019, Northwood Inc., an independent company that manages the DME, P&O and medical supply provider network for Medicare Plus Blue PPO members, will also handle authorizations, utilization management and claims processing. Northwood- contracted providers will be required to obtain authorizations and submit their claims to Northwood. In the next few months, Northwood will send provider education communication materials to its contracted providers with details on the transition and information about handling authorizations, utilization management and claims for Medicare Plus Blue members. For more information, see the February 2019 issue of The Record. Procedure code *87798 will require supportive documentation Effective March 1, 2019, Blue Cross will require identification of the organism being tested and/or supportive documentation when a claim for laboratory procedure code *87798 (not-otherwise-classified) is submitted. For more information, refer to the Claims chapter of the Blue Cross PPO (commercial) Provider Manual (Medical records and other claim attachments > Services that Always Require Medical Records). *CPT codes, descriptions and two-digit numeric modifiers only are copyright 2018 American Medical Association. All rights reserved. |
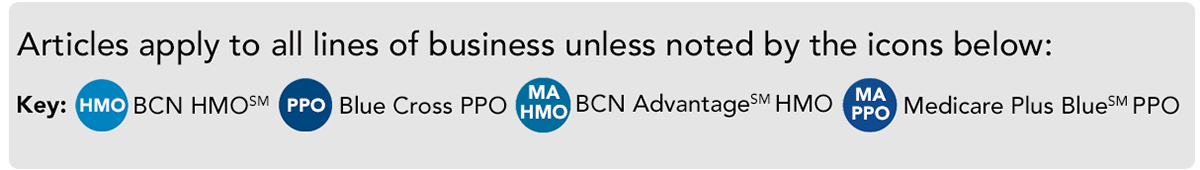
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. |