
Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
June 2024
Emergency Department Claim Analyzer reminder and reconsideration programAs a reminder, the Emergency Department Claim Analyze, or EDCA, program was re-implemented on June 1, 2024, in conjunction with a new Emergency Department Facility Evaluation and Management reimbursement policy. This reimbursement policy was developed to ensure that facilities are reimbursed based on the consistent coding that correctly describes the patient’s clinical condition and the health care services provided in accordance with industry standards and Centers for Medicare & Medicaid Services guidelines. What does this mean to hospitals? Blue Cross is reviewing evaluation and management, or E/M, claims that are billed with a level four or five E/M code (*99284 or *99285) for the appropriate level of care on a prepayment basis. Claims that don't meet the policy criteria will be adjusted and reimbursed at the appropriate level. At this time, claims that are two or more levels higher than the Blue Cross reimbursement policy will be adjusted. Claims that are one level higher won't be adjusted. Blue Cross will continue to monitor all emergency department claims submitted. We reserve the right to modify the scope if adherence and adjustments don't align with the reimbursement policy. Hospitals reimbursed by the fee schedule For hospitals reimbursed via the fee schedule, claims recommended for adjustment will be adjusted to the appropriate level. These claims will be paid according to the fee schedule requiring no additional action by the hospitals. The change will be reflected in the provider voucher and 835 electronic transaction. This will also be shown with a CO186 adjustment code, level of care change adjustment. Hospitals reimbursed by percent of charge For hospitals reimbursed percent of charge, emergency department claims recommended for adjustment will be denied. Remittance will be provided with information on how to be reimbursed and will indicate the appropriate level recommended for approval. It will require hospitals to adjust the claim and charges associated and re-submit to Blue Cross for processing and payment. What should I do if I am a percent of charge hospital, and my claim was denied? You can submit a corrected claim through either:
What should I do if I disagree with the claim adjustment? Providers who disagree with the claim adjustment have the right to submit a reconsideration request to have their claim reviewed. To have the claim reviewed, providers must supply:
If these items aren't provided, the claim will remain adjusted/denied and the reconsideration will be upheld. To submit a reconsideration using Availity, please complete the following steps:
Note: If you want to initiate appeals on additional claims, click Close to return to the Claim Status results page. To continue your appeal of the claim in question, complete the additional steps outlined here. 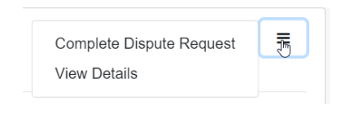 Important: In the field shown below, enter this information: 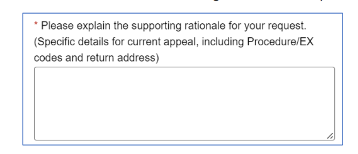 The Emergency Department Facility Evaluation and Management Reimbursement Policy can be found on the Provider Resources website:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. |
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|