Medicare Advantage Prior Authorization
Blue Cross Blue Shield of Michigan and Blue Care Network require prior authorization for certain benefits. This means we need to review a service to be sure it is medically necessary and appropriate.
If a prior authorization is required for your medical service, your doctor or health care professional must submit the prior authorization request. Once we get the request and supporting medical records, we will begin the review process.
Do you need prior authorization?
Services summary
If you have a Medicare Plus Blue℠ PPO, BCN Advantage℠ HMO or BCN Advantage℠ HMO-POS plan, our Procedure codes for which providers must request prior authorization (PDF) shows the services that require prior authorization before you receive them.
A prior authorization is not a guarantee of benefits or payment. Please check your member eligibility and benefits and medical policy coverage guidelines.
Clinical review criteria
Blue Cross and BCN use evidence-based clinical standards of care to help determine whether a benefit may be covered under the member’s health plan.
Medical policies follow Medicare Advantage Medical Policy Guidelines to comply with the Centers for Medicare & Medicaid Services (CMS) Policy, National Coverage Determinations (NCDs), and /or Local Coverage Determinations (LCDs). The criteria to determine if a service is medically necessary can be accessed on our Medical Policy Router Search page and in additional criteria.
See the Medicare Coverage Database* for the most current NCD, LCD, Local Coverage Articles (LCAs) and CMS Online Manual System/Transmittals.
Additional information on specific certain procedures is available in Preview questionnaires and medical necessity criteria (PDF).
Prior authorization requests
Prior authorization requests managed by BCBSM and BCNA of medical and surgical services
Blue Cross and BCN use the following:
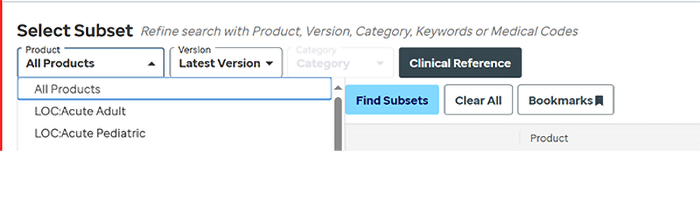
- For acute medical and surgical inpatient requests: Nationally recognized InterQual® medical necessity criteria select:
- LOC: Acute Adult
- LOC: Acute Pediatric
- Note: Surgical procedures follow the CMS Inpatient Only List Addendum E:
- Accessible through the InterQual criteria, under Clinical Reference as a PDF.
- For post-acute care requests: InterQual criteria for initial screening of requests and CMS criteria to make final determinations select:
- LOC: Long-Term Acute Care
- LOC: Inpatient Rehabilitation
- LOC: Subacute/SNF
- For select elective inpatient and outpatient services select:
- CP: Procedures
Sign up or log in to One Healthcare ID to view InterQual criteria for medical and surgical services.
Providers/Members should select a “Product” under the Select Subset menu to view criteria.
Behavioral Health Services (effective Jan. 1, 2024)
Blue Cross Behavioral HealthSM manages behavioral health prior authorizations and case management services for Medicare Plus Blue and BCN Advantage members. The medical necessity criteria used are the same for all members.
The following guidelines are used for all lines of business:
- Level of Care Utilization System (LOCUS) (PDF) - To evaluate behavioral health treatment requests for adults age 19+
- Child and Adolescent Level of Care Utilization System (CALOCUS) (PDF) - To evaluate mental health treatment requests for children and adolescents ages 6 – 18 years
- Early Childhood Service Intensity Instrument (ECSII) (PDF) - To evaluate mental health treatment requests for infants, toddlers, and children ages birth through 5 years
- ASAM Criteria (PDF) - To evaluate substance use disorder service and treatment requests for dates of service from April 1, 2023, through March 31, 2024
- The ASAM Criteria, Fourth Edition - To evaluate substance use disorder service and treatment requests for dates of service on or after April 1, 2024. Scroll to the “What’s new in The ASAM Criteria, Fourth Edition?” section.
- Applied Behavior Analysis
- Applied Behavior Analysis (ABA) Supplemental Policy (PDF) – For dates of service on or after Jan. 1, 2026
- Applied Behavior Analysis (ABA) Supplemental Policy (PDF) — For dates of service from April 22, 2025, through Dec. 31, 2025
- Applied Behavior Analysis (ABA) Supplemental Policy (PDF) — For dates of service from Jan. 1, 2024, through April 21, 2025
Outside review of prior authorization requests
Prior authorization requests for certain types of services are sometimes reviewed by outside vendors.
- Cardiology: Carelon Medical Benefits Management Cardiology Guidelines
- Echocardiogram: Carelon Imaging of the Heart
- High-tech radiology: Carelon Radiology Guidelines
- Musculoskeletal services: TurningPoint Healthcare Solutions
- Proton beam therapy: Carelon Proton Beam Therapy
- PT, OT, ST (BCN Advantage members only): EviCore by Evernorth® Musculoskeletal Therapies
- Radiation oncology: EviCore Radiation Oncology Solution
Additional information for providers
Before providing services, make sure you check benefits and eligibility and medical policy coverage guidelines, using the self-service tools on Availity EssentialsTM.
If you have questions, please contact Provider Inquiry from 8:30 a.m. to noon or 1 to 5 p.m., Monday through Friday:
- Professional: 1-800-344-8525
- Facility: 1-800-249-5103
*Blue Cross and BCN do not own or control this website.
Availity® is an independent company that contracts with Blue Cross and BCN to offer provider portal and electronic data interchange services.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
EviCore by Evernorth is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.